Understanding flu vaccine hesitancy in Liverpool’s ethnically diverse communities
November 27, 2025
November 27, 2025
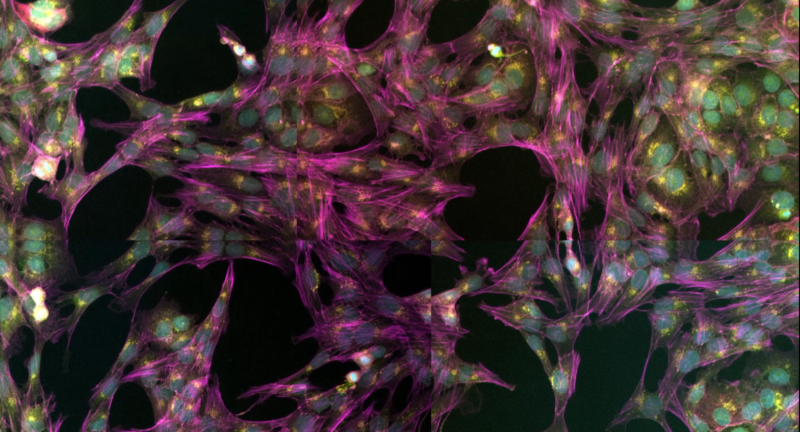
A strategic research post funded by The Pandemic Institute is helping scientists deepen their understanding of some of the world’s most dangerous viruses while strengthening the UK’s preparedness for future pandemics. The post, held by Dr Tessa Prince, focuses on combining artificial intelligence and advanced microscopy to create new ways of studying high-risk viruses. Tessa’s…
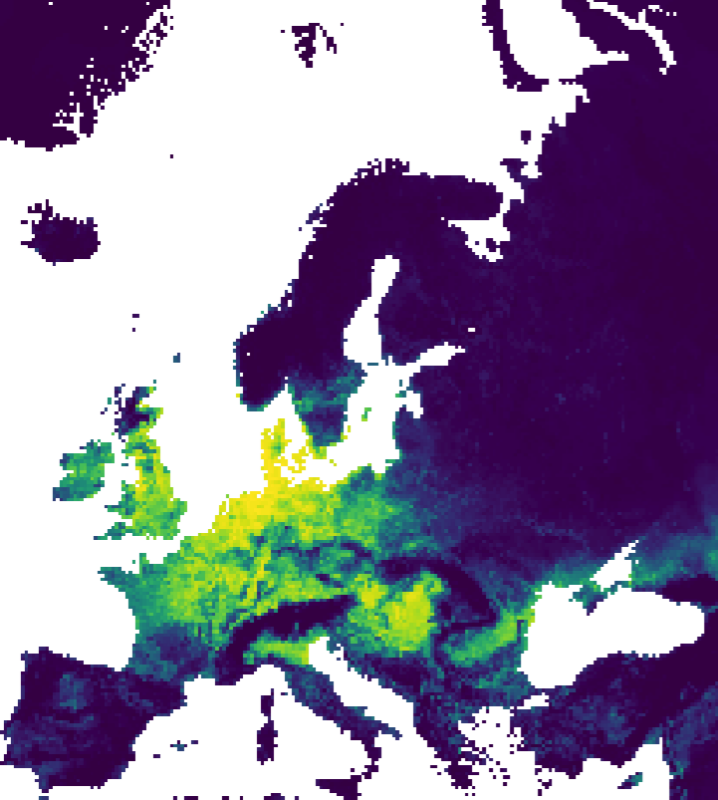
A study funded through a partnership between The Pandemic Institute and CSL Seqirus has been published in Scientific Reports. The research maps bird flu risk across Europe and, unlike earlier studies that focused mainly on landscape and climate, it also uses information about wild bird populations and how they interact with their environment. Bird flu,…